When a diagnostic kit reaches a clinician or a point-of-care test station, the end user expects one thing above all: consistent, trustworthy results. For antigen-detection tests — especially for high-impact targets like Dengue NS1 and Hepatitis B surface antigen (HBsAg), that trust depends almost entirely on the quality of the antibody pairs used in the assay.
Validated antibody pairs are not just reagents. They are engineered building blocks that determine assay sensitivity, specificity, stability, and ultimately clinical value. In this article we unpack the technical reasons why certain antibody pairs become reliable, how they are validated, what regulatory and field realities matter for Dengue NS1 and HBsAg assays, and how a partner like deNOVO Biolabs supports diagnostic manufacturers with ready-to-use and custom validated pairs.
Why Dengue NS1 and HBsAg matter?
Dengue and hepatitis B are high-priority public health challenges that rely heavily on accurate diagnostic testing.
- Dengue: The World Health Organization estimates tens of millions of symptomatic dengue infections annually worldwide and warns of expanding geographical spread. Reliable early detection (often via NS1 antigen tests) is essential for patient triage and outbreak response. See WHO Dengue facts for context.
(WHO dengue: https://www.who.int/health-topics/dengue) - Hepatitis B (HBsAg): The WHO estimates nearly 296 million people living with chronic hepatitis B infection globally (2020 data). Early detection of HBsAg is critical for linkage to care and prevention of liver disease. WHO hepatitis B: https://www.who.int/news-room/fact-sheets/detail/hepatitis-b
Because both pathogens have large public-health footprints, assay reliability carries real consequences — missed diagnoses or false positives can impact patient outcomes and public health responses.
What is an antibody pair?
In a sandwich immunoassay (ELISA or lateral flow), two antibodies are paired:
- A capture antibody, immobilized on the test matrix, that binds the target antigen; and
- A detection antibody, typically labeled (enzyme, colloidal gold, fluorophore), that binds a different epitope on the same antigen to produce signal.
A validated antibody pair is one in which both antibodies have been selected, optimized, and tested together across relevant performance parameters: affinity, specificity, epitope compatibility, cross-reactivity, stability, and lot-to-lot reproducibility. Validation ensures the pair performs not only in clean lab buffers but also in real biological matrices (serum, plasma, whole blood) and under expected field conditions.
Core technical characteristics of reliable antibody pairs
Below are the technical attributes that define a reliable antibody pair for Dengue NS1 and HBsAg testing.
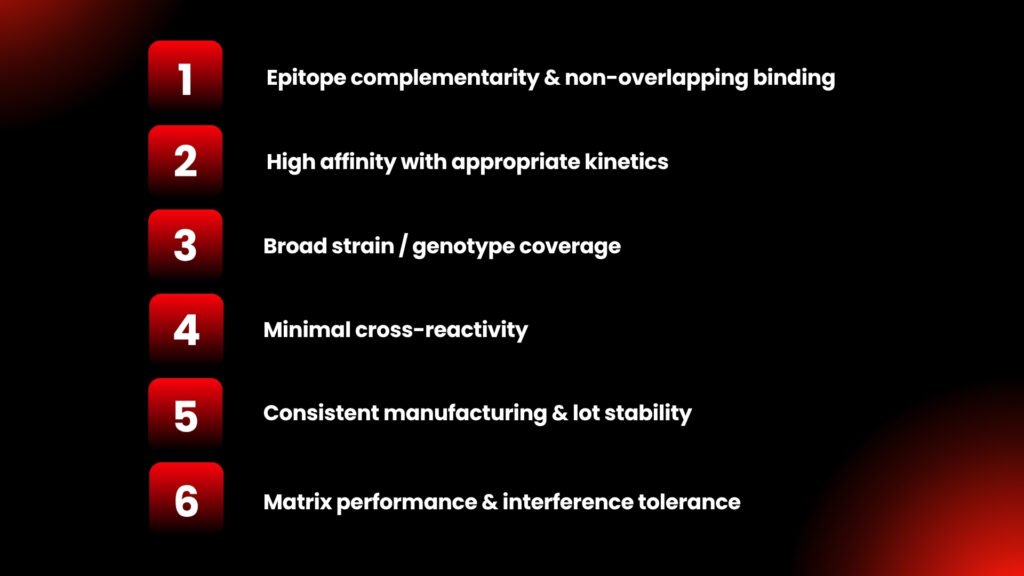
1. Epitope complementarity & non-overlapping binding
A great pair binds to distinct, non-competing epitopes so capture and detection don’t sterically block one another. Epitope mapping (peptide mapping, mutational analysis) verifies spatial compatibility.
2. High affinity with appropriate kinetics
Affinity (KD) and on/off rates affect sensitivity. High-affinity capture can improve retention of low antigen levels; detection antibodies with rapid on-rates produce stronger early signals. However, optimum kinetics depend on assay format (LFA vs ELISA).
3. Broad strain / genotype coverage
Dengue has four serotypes (DENV-1 to DENV-4). HBsAg has variants across genotypes. Reliable pairs are vetted against multiple serotypes/genotypes or are raised against conserved regions to ensure broad detection.
4. Minimal cross-reactivity
Cross-reactivity — with other flaviviruses (for dengue) or with non-HBs proteins — reduces specificity. Rigorous cross-reactivity testing against panels of related pathogens, heterophile antibodies, and common interferents is mandatory.
5. Consistent manufacturing & lot stability
Monoclonal or recombinant antibodies provide lot-to-lot consistency more readily than polyclonal reagents. Stability under storage and transport conditions must be proven by accelerated and real-time stability studies.
6. Matrix performance & interference tolerance
Real patient samples contain lipids, heterophile antibodies, bilirubin, hemoglobin, etc. Reliable pairs maintain performance (recovery, linearity) in the intended sample matrix.
Validation workflow
A validated pair goes through multiple steps:
- Antigen selection & design — recombinant or native antigen for immunization and screening (for NS1, properly folded recombinant NS1 is essential).
- Immunization and clone generation (monoclonals) or polyclonal production if appropriate.
- Primary screening for binding to antigen (ELISA, SPR).
- Pair screening — testing candidate capture and detection combinations in assay formats (ELISA, LFA prototypes).
- Cross-reactivity panels & interference testing — including related pathogens and common blood interferents.
- Matrix testing & spike recovery — assessing recovery across representative clinical samples.
- Precision & reproducibility — intra- and inter-assay CV, lot-to-lot studies.
- Stability studies — accelerated and real-time.
- Clinical correlation / field testing — final verification against a reference or RT-PCR (for dengue) or gold-standard serology (for HBsAg).
- Regulatory documentation — Certificates of Analysis, validation reports, and data required for regulatory submission.
At deNOVO Biolabs, each of these steps is performed with traceable SOPs and documented QC checkpoints, so partners receive not only reagents but regulatory-ready data packages (see services and contact pages for details).
Dengue NS1
NS1 is a secreted, glycosylated viral protein detectable early in the disease course (first 1–5 days). Its key assay considerations:
- Serotype variability: NS1 epitopes vary across the four dengue serotypes, meaning your antibody pair must either be cross-reactive across serotypes or you must accept differential sensitivity. See reviews on NS1 assay sensitivity on PubMed.
- Sensitivity window: NS1 assays are most effective during early infection; detection sensitivity depends on antibody affinity and antigen abundance in the given population.
- Cross-reactivity with other flaviviruses: In regions where dengue co-circulates with Zika or Yellow Fever, specificity testing is crucial. Cross-reactivity can be mitigated by epitope selection during antibody development.
Performance benchmarks to expect (typical ranges reported in literature and manufacturers’ data): NS1 assay sensitivity often varies between ~60–95% depending on serotype and timing; specificity is typically >90% when validated correctly.
HBsAg
HBsAg detection is central to diagnosing hepatitis B infection and is commonly used in blood screening and patient diagnosis.
- Genotype variation: HBsAg subtypes/genotypes influence epitope availability. Reliable antibody pairs are tested across genotypes (A–J) to ensure broad detection.
- Surface antigen forms: HBsAg exists as different particle forms (small, medium, large surface proteins); antibodies targeting conserved regions that appear on circulating particles ensure better clinical sensitivity.
- Window period & mutant strains: Detection of escape mutants or low-titer infections requires high sensitivity and broad epitope targeting.
Performance expectations: High-quality HBsAg assays achieve clinical sensitivity and specificity typically >99% in blood-screening contexts when using validated antibody pairs and state-of-the-art assay design.
Choosing between monoclonal, polyclonal & recombinant antibody
- Monoclonal antibodies:
Provide specificity and reproducibility; preferred for long-term production and regulated assays. - Polyclonal antibodies:
Offer high signal and multi-epitope binding; useful for early screening or where antigen variability is extreme. However, batch variability is a concern for commercialization. - Recombinant antibodies:
Offer traceability, sequence definition, and unlimited reproducible production — increasingly the industry standard for regulated diagnostic assays.
deNOVO’s practice: we recommend and supply monoclonal or recombinant monoclonal pairs for final products and may use polyclonal reagents during exploratory stages for high signal detection.
Practical checklist ✅
Before signing a supplier or moving to scale, use this practical checklist:
- Epitope mapping report — confirmed non-overlapping epitopes.
- Affinity & kinetics (SPR/BLI) — KD and on/off rates provided.
- Cross-reactivity panel — tests against related pathogens and human interferents.
- Matrix recovery & spike tests — serum/plasma/whole blood as applicable.
- Precision data — intra/inter-assay CVs across ≥3 runs.
- Stability & shelf-life — accelerated and real-time data.
- Lot-to-lot comparison — at least 2+ independent lots tested.
- Field/clinical correlation — head-to-head testing vs reference methods (PCR or gold-standard serology).
- Documentation pack — CoA, SDS, validation reports for regulatory filing.
- Supply & scale assurance — manufacturing capacity and lead times.
Regulatory & Quality considerations
Regulatory authorities expect robust validation and traceability. For IVDs, guidance from regulators (FDA/EMA/WHO) stresses product-specific validation and clear documentation of clinical performance. Link to FDA guidance on analytical validation for bioanalytical methods: https://www.fda.gov.
For blood screening and clinical-grade diagnostics the bar is particularly high; partnering with a reagent supplier that has documented QC systems, batch traceability, and regulatory support greatly simplifies product clearance.
Want to evaluate validated antibody pairs for your Dengue NS1 or HBsAg assay?
Request a free feasibility call and receive a custom validation plan: Book a technical call →